Pattern of Rise in Intraocular Pressure Following Nd: Yag Laser Posterior Capsulotomy
Keywords:
Posterior Capsular Opacification, Nd:YAG Capsulotomy, Intraocular Pressure, Laser Energy, Glaucoma Prophylaxis, Pseudophakia.Abstract
Background: Posterior capsular opacification (PCO) remains the most common delayed cause of visual decline after cataract surgery. Nd:YAG laser posterior capsulotomy restores the visual axis but can precipitate transient intraocular pressure (IOP) elevation. The necessity and scope of prophylactic anti-glaucoma therapy in routine practice—particularly as a function of delivered laser energy—remain debated.
Methods: In a prospective observational study at a tertiary eye care center (November 2023–September 2025), 87 pseudophakic eyes with visually significant PCO underwent Nd:YAG capsulotomy; fellow eyes served as controls. No prophylactic anti-glaucoma medication was administered. IOP (non-contact tonometry) was recorded at baseline and 0.5, 1, 2, 3, 4, and 24 hours post-procedure. Total laser energy (mJ) was computed as pulse energy × number of pulses. “Significant IOP rise” was predefined as ≥6 mmHg from baseline in the treated eye or an inter-eye difference ≥6 mmHg. Associations with energy, age, and sex were analyzed (t-test, chi-square; p<0.05).
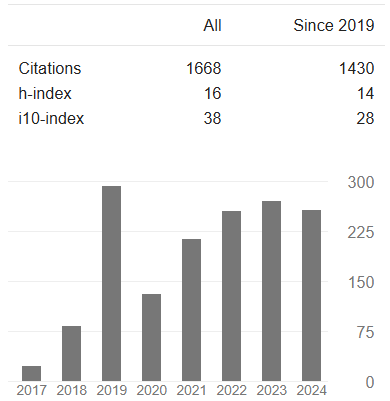
Results: Significant IOP rise occurred in 16/87 eyes (18.4%). The mean onset of the spike was 1.4 hours (range 0.5–3.0), with 62.5% peaking at 1 hour. In the spike cohort, the mean magnitude was 7.5 mmHg (range 6–14); one eye reached 30.4 mmHg and received oral acetazolamide. By 24 hours, 87.5% of spikes had resolved; two eyes required observation up to 48 hours. Higher total energy correlated with IOP elevation (t=2.688; p=0.009). Incidence rose with energy strata: 8.3% (<21 mJ), 25.0% (21–40 mJ), and 45.5% (>40 mJ). Age and sex showed no significant associations.
Conclusion: Post-Nd: YAG capsulotomy IOP spikes are infrequent, early, and typically self-limited, but their risk increases with higher total energy. A pragmatic protocol is suggested: no prophylaxis for <21 mJ; a 1-hour post-procedure IOP check for 21–40 mJ; and immediate anti-glaucoma treatment when >40 mJ or if the measured IOP is elevated. Multi-session, low-energy strategies may further mitigate risk.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Authors

This work is licensed under a Creative Commons Attribution 4.0 International License.